Overview
Over-pronation, or flat feet, is a common biomechanical problem that occurs in the walking process when a person's arch collapses upon weight bearing. This motion can cause extreme stress or inflammation on the plantar fascia, potentially causing severe discomfort and leading to other foot problems.
Causes
There are many possible causes for overpronation, but researchers have not yet determined one underlying cause. Hintermann states, Compensatory overpronation may occur for anatomical reasons, such as a tibia vara of 10 degrees or more, forefoot varus, leg length discrepancy, ligamentous laxity, or because of muscular weakness or tightness in the gastrocnemius and soleus muscles. Pronation can be influenced by sources outside of the body as well. Shoes have been shown to significantly influence pronation. Hintermann states that the same person can have different amounts of pronation just by using different running shoes. It is easily possible that the maximal ankle joint eversion movement is 31 degrees for one and 12 degrees for another running shoe.
Symptoms
In addition to problems overpronation causes in the feet, it can also create issues in the calf muscles and lower legs. The calf muscles, which attach to the heel via the Achilles tendon, can become twisted and irritated as a result of the heel rolling excessively toward the midline of the body. Over time this can lead to inflexibility of the calf muscles and the Achilles tendon, which will likely lead to another common problem in the foot and ankle complex, the inability to dorsiflex. As such, overpronation is intrinsically linked to the inability to dorsiflex.
Diagnosis
So, how can you tell if you have overpronation, or abnormal motion in your feet, and what plantar fasciitis treatment will work to correct it? Look at your feet. While standing, do you clearly see the arch on the inside of your foot? If not, and if the innermost part of your sole touches the floor, then your feet are overpronated. Look at your (running/walking) shoes. If your shoes are more worn on the inside of the sole in particular, then pronation may be a problem for you. Use the wet foot test. Wet your feet and walk along a section of pavement, then look at the footprints you leave behind. A normal foot will leave a print of the heel connected to the forefoot by a strip approximately half the width of the foot on the outside of the sole. If you?re feet are pronated there may be little distinction between the rear and forefoot.
Non Surgical Treatment
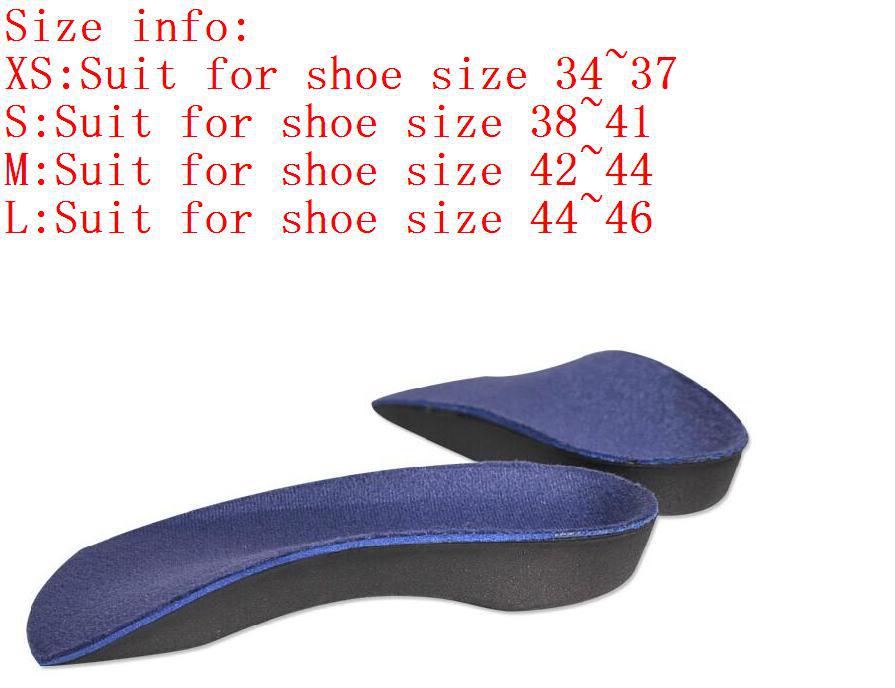
Personal orthotics can be prescribed via your healthcare professional. If finances or insurance are issues, similar and often better options can be purchased online for overpronation. The right walking shoes are also essential. Most shoes cater to neutral foot gaits, unless they specifically state otherwise. That won?t help you if your foot rolls inward. In order to correct the issue, you need shoes with stability or motion control abilities, low heels, deep heel cups, and good arch support.
Prevention
With every step we take, we place at least half of our body weight on each foot (as we walk faster, or run, we can exert more than twice our body weight on each foot). As this amount of weight is applied to each foot there is a significant shock passed on to our body. Custom-made orthotics will absorb some of this shock, helping to protect our feet, ankles, knees, hips, and lower back.
Over-pronation, or flat feet, is a common biomechanical problem that occurs in the walking process when a person's arch collapses upon weight bearing. This motion can cause extreme stress or inflammation on the plantar fascia, potentially causing severe discomfort and leading to other foot problems.

Causes
There are many possible causes for overpronation, but researchers have not yet determined one underlying cause. Hintermann states, Compensatory overpronation may occur for anatomical reasons, such as a tibia vara of 10 degrees or more, forefoot varus, leg length discrepancy, ligamentous laxity, or because of muscular weakness or tightness in the gastrocnemius and soleus muscles. Pronation can be influenced by sources outside of the body as well. Shoes have been shown to significantly influence pronation. Hintermann states that the same person can have different amounts of pronation just by using different running shoes. It is easily possible that the maximal ankle joint eversion movement is 31 degrees for one and 12 degrees for another running shoe.
Symptoms
In addition to problems overpronation causes in the feet, it can also create issues in the calf muscles and lower legs. The calf muscles, which attach to the heel via the Achilles tendon, can become twisted and irritated as a result of the heel rolling excessively toward the midline of the body. Over time this can lead to inflexibility of the calf muscles and the Achilles tendon, which will likely lead to another common problem in the foot and ankle complex, the inability to dorsiflex. As such, overpronation is intrinsically linked to the inability to dorsiflex.
Diagnosis
So, how can you tell if you have overpronation, or abnormal motion in your feet, and what plantar fasciitis treatment will work to correct it? Look at your feet. While standing, do you clearly see the arch on the inside of your foot? If not, and if the innermost part of your sole touches the floor, then your feet are overpronated. Look at your (running/walking) shoes. If your shoes are more worn on the inside of the sole in particular, then pronation may be a problem for you. Use the wet foot test. Wet your feet and walk along a section of pavement, then look at the footprints you leave behind. A normal foot will leave a print of the heel connected to the forefoot by a strip approximately half the width of the foot on the outside of the sole. If you?re feet are pronated there may be little distinction between the rear and forefoot.

Non Surgical Treatment
Personal orthotics can be prescribed via your healthcare professional. If finances or insurance are issues, similar and often better options can be purchased online for overpronation. The right walking shoes are also essential. Most shoes cater to neutral foot gaits, unless they specifically state otherwise. That won?t help you if your foot rolls inward. In order to correct the issue, you need shoes with stability or motion control abilities, low heels, deep heel cups, and good arch support.
Prevention
With every step we take, we place at least half of our body weight on each foot (as we walk faster, or run, we can exert more than twice our body weight on each foot). As this amount of weight is applied to each foot there is a significant shock passed on to our body. Custom-made orthotics will absorb some of this shock, helping to protect our feet, ankles, knees, hips, and lower back.

 Complete Achilles tendon ruptures occur most commonly at the mid-substance, but also distally at the insertion site or proximally at the myotendinous junction. These can be traumatic and devastating injuries, resulting in significant pain, disability, and healthcare cost. As many as 2.5 million individuals sustain Achilles tendon ruptures each year and the incidence is rising. This trend is due, in part, to an increase in athletic participation across individuals of all ages. Causes Your Achilles tendon helps you point your foot downward, rise on your toes and push off your foot as you walk. You rely on it virtually every time you move your foot. Rupture usually occurs in the section of the tendon located within 2 1/2 inches (about 6 centimeters) of the point where it attaches to the heel bone. This section may be predisposed to rupture because it gets less blood flow, which also may impair its ability to heal. Ruptures often are caused by a sudden increase in the amount of stress on your Achilles tendon. Common examples include increasing the intensity of sports participation, especially in sports that involve jumping, falling from a height, stepping into a hole. Symptoms Patients with an Achilles tendon rupture frequently present with complaints of a sudden snap in the lower calf associated with acute, severe pain. The patient reports feeling like he or she has been shot, kicked, or cut in the back of the leg, which may result in an inability to ambulate further. A patient with Achilles tendon rupture will be unable to stand on his or her toes on the affected side. Diagnosis A staggering 20%-30% of Achilles tendon ruptures are missed. Thompson (calf squeeze) test is 96% sensitive and 93% sensitive. Unfortunately, some health practitioners fail to perform this simple clinical test. Ultrasound examination or an MRI can confirm an Achilles tendon rupture. Non Surgical Treatment A medical professional will take MRI scans to confirm the diagnosis and indicate the extent of the injury. Sometimes the leg is put in a cast and allowed to heal without surgery. This is generally not the preferred method, particularly for young active people. Surgery is the most common treatment for an achilles tendon rupture.
Complete Achilles tendon ruptures occur most commonly at the mid-substance, but also distally at the insertion site or proximally at the myotendinous junction. These can be traumatic and devastating injuries, resulting in significant pain, disability, and healthcare cost. As many as 2.5 million individuals sustain Achilles tendon ruptures each year and the incidence is rising. This trend is due, in part, to an increase in athletic participation across individuals of all ages. Causes Your Achilles tendon helps you point your foot downward, rise on your toes and push off your foot as you walk. You rely on it virtually every time you move your foot. Rupture usually occurs in the section of the tendon located within 2 1/2 inches (about 6 centimeters) of the point where it attaches to the heel bone. This section may be predisposed to rupture because it gets less blood flow, which also may impair its ability to heal. Ruptures often are caused by a sudden increase in the amount of stress on your Achilles tendon. Common examples include increasing the intensity of sports participation, especially in sports that involve jumping, falling from a height, stepping into a hole. Symptoms Patients with an Achilles tendon rupture frequently present with complaints of a sudden snap in the lower calf associated with acute, severe pain. The patient reports feeling like he or she has been shot, kicked, or cut in the back of the leg, which may result in an inability to ambulate further. A patient with Achilles tendon rupture will be unable to stand on his or her toes on the affected side. Diagnosis A staggering 20%-30% of Achilles tendon ruptures are missed. Thompson (calf squeeze) test is 96% sensitive and 93% sensitive. Unfortunately, some health practitioners fail to perform this simple clinical test. Ultrasound examination or an MRI can confirm an Achilles tendon rupture. Non Surgical Treatment A medical professional will take MRI scans to confirm the diagnosis and indicate the extent of the injury. Sometimes the leg is put in a cast and allowed to heal without surgery. This is generally not the preferred method, particularly for young active people. Surgery is the most common treatment for an achilles tendon rupture.  Surgical Treatment The goal of surgery is to realign the two ends of the ruptured tendon to allow healing. There are multiple techniques to accomplish this goal that will vary from surgeon to surgeon. Recovery from this injury is usually very successful with return to full function in approximately 6 months. Post operatively casting is required with the use of crutches or other means to remain non-weightbearing for 4-8 weeks. This is followed by a course of physical therapy. Partial rupture may or may not require surgical intervention depending on the extent of injury but cast immobilization is a common requirement. Prevention To prevent Achilles tendonitis or rupture, the following tips are recommended. Avoid activities that place an enormous stress on the heel (for example, uphill running or excessive jumping). Stop all activity if there is pain at the back of the heel. If pain resumes with one particular exercise, another exercise should be selected. Wear proper shoes. Gradually strengthen calf muscles with sit-ups if prior episodes of Achilles tendonitis have occurred. Always warm up with stretching exercises before any activity. Avoid high-impact sports if prior episodes of Achilles tendon injury.
Surgical Treatment The goal of surgery is to realign the two ends of the ruptured tendon to allow healing. There are multiple techniques to accomplish this goal that will vary from surgeon to surgeon. Recovery from this injury is usually very successful with return to full function in approximately 6 months. Post operatively casting is required with the use of crutches or other means to remain non-weightbearing for 4-8 weeks. This is followed by a course of physical therapy. Partial rupture may or may not require surgical intervention depending on the extent of injury but cast immobilization is a common requirement. Prevention To prevent Achilles tendonitis or rupture, the following tips are recommended. Avoid activities that place an enormous stress on the heel (for example, uphill running or excessive jumping). Stop all activity if there is pain at the back of the heel. If pain resumes with one particular exercise, another exercise should be selected. Wear proper shoes. Gradually strengthen calf muscles with sit-ups if prior episodes of Achilles tendonitis have occurred. Always warm up with stretching exercises before any activity. Avoid high-impact sports if prior episodes of Achilles tendon injury.
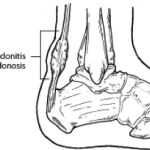 The Achilles tendon connects the muscles in the back of your calf to your heel bone. There are two basic variations of Achilles injuries. Achilles tendonitis, and a complete tear. Its important to know whether the Achilles is torn or not, because the treatment is very different, a torn Achilles may require surgery. Achilles tendonitis probably means rehab and rest. While tendonitis is a gradual onset of pain that tends to get worse with more activity, an Achilles tear is a sudden injury, and it feels as if you were hit or kicked in the back of the ankle. A tear usually affects your ability to walk properly. Because an Achilles tendon rupture can impair your ability to walk, its common to seek immediate treatment. You may also need to consult with doctors specializing in sports medicine or orthopaedic surgery.
The Achilles tendon connects the muscles in the back of your calf to your heel bone. There are two basic variations of Achilles injuries. Achilles tendonitis, and a complete tear. Its important to know whether the Achilles is torn or not, because the treatment is very different, a torn Achilles may require surgery. Achilles tendonitis probably means rehab and rest. While tendonitis is a gradual onset of pain that tends to get worse with more activity, an Achilles tear is a sudden injury, and it feels as if you were hit or kicked in the back of the ankle. A tear usually affects your ability to walk properly. Because an Achilles tendon rupture can impair your ability to walk, its common to seek immediate treatment. You may also need to consult with doctors specializing in sports medicine or orthopaedic surgery.
