Overview

If you have flat feet, you may also experience pain throughout the lower body and into the lower back. Orthotics can be prescribed to create a system of support for the body and surgery can also offer a more permanent solution. Contact us today to discuss which treatment option may be right for you.
Causes
A Rigid Flat Foot may be congenital, where the arch never develops when growing. A Rigid Flat Foot can also be acquired due to disease processes involving inflammatory arthritis, neurological conditions such as Charcot neuro-arthropathy or trauma. A Flexible Flat Foot (fallen arches) may also be congenital where excessive pronation occurs for shock absorption. In some cases this condition may be the result of neurological disease or injury involving muscle weakness, hyper-mobile joints or ligament laxity. These conditions may allow for excessive pronation causing the arch to fall when weight bearing or during activity. Both of these foot types can result in posture mal-alignment involving the lower back, hips, knees and feet which may result in pain in those areas.
Symptoms
Fallen arches may induce pain in the heel, the inside of the arch, the ankle, and may even extend up the body into the leg (shin splints), knee, lower back and hip. You may also experience inflammation (swelling, redness, heat and pain) along the inside of the ankle (along the posterior tibial tendon). Additionally, you may notice some changes in the way your foot looks. Your ankle may begin to turn inward (pronate), causing the bottom of your heel to tilt outward. Other secondary symptoms may also show up as the condition progresses, such as hammertoes or bunions. You may also want to check your footprint after you step out of the shower. (It helps if you pretend you?re in a mystery novel, and you?re leaving wet, footprinty clues that will help crack the case.) Normally, you can see a clear imprint of the front of your foot (the ball and the toes) the heel, and the outside edge of your foot. There should be a gap (i.e. no footprinting) along the inside where your arches are. If your foot is flat, it?ll probably leave an imprint of the full bottom of your foot-no gap to be had. Your shoes may also be affected: because the ankle tilts somewhat with this condition, the heel of your shoes may become more worn on one side than another.
Diagnosis
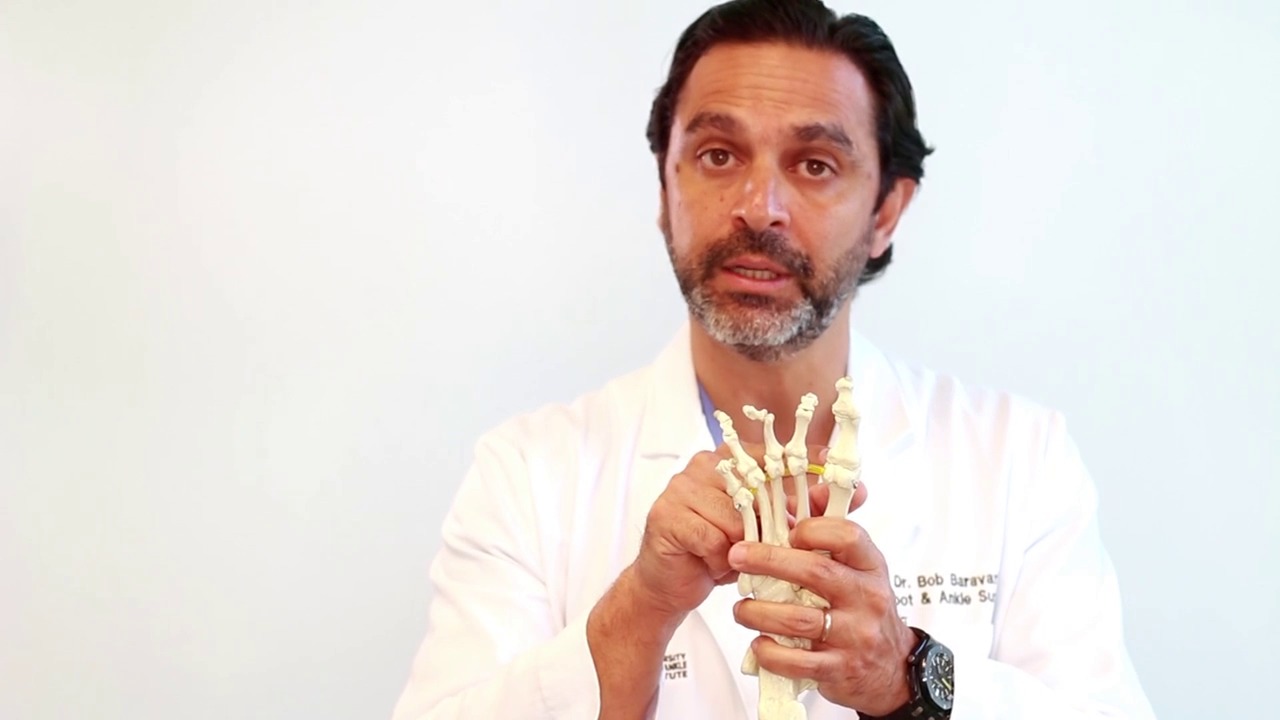
Podiatrists are trained in expertly assessing flat feet and identifying different risk factors and the causes for it. Initial assessment will begin with a detailed history attempting to find out if any underlying illness has resulted in this. A detailed clinical examination normally follows. The patient may be asked to perform certain movements such as walking or standing on their toes to assess the function of the foot. Footwear will also be analysed to see if there has been excessive wear or if they are contributing to the pronation of the foot. To assess the structure of the foot further, the podiatrist may perform certain x-rays to get a detailed idea of the way the bones are arranged and how the muscle tissues may be affecting them. It also helps assess any potential birth defects in a bit more detail.
pes planus radiology
Non Surgical Treatment
If you have flat feet, you may also experience pain throughout the lower body and into the lower back. Orthotics (custom-made rigid foot supports) can be prescribed when over-the-counter supports do not provide releif and surgery can also offer a more permanent solution in severe cases. The board-certified doctors in our practice would be able to select the most appropriate course of action in each case.
Surgical Treatment

Surgical procedures for flat feet vary depending on the root cause of the condition. Surgical correction to control pronation may include bone implants or Achilles tendon lengthening. Tendon transfer, which is a procedure to re-attach a tendon to another area of bone, may also be used to reduce pronation and improve foot function.
Prevention
Well-fitted shoes with good arch support may help prevent flat feet. Maintaining a healthy weight may also lower wear and tear on the arches.

If you have flat feet, you may also experience pain throughout the lower body and into the lower back. Orthotics can be prescribed to create a system of support for the body and surgery can also offer a more permanent solution. Contact us today to discuss which treatment option may be right for you.
Causes
A Rigid Flat Foot may be congenital, where the arch never develops when growing. A Rigid Flat Foot can also be acquired due to disease processes involving inflammatory arthritis, neurological conditions such as Charcot neuro-arthropathy or trauma. A Flexible Flat Foot (fallen arches) may also be congenital where excessive pronation occurs for shock absorption. In some cases this condition may be the result of neurological disease or injury involving muscle weakness, hyper-mobile joints or ligament laxity. These conditions may allow for excessive pronation causing the arch to fall when weight bearing or during activity. Both of these foot types can result in posture mal-alignment involving the lower back, hips, knees and feet which may result in pain in those areas.
Symptoms
Fallen arches may induce pain in the heel, the inside of the arch, the ankle, and may even extend up the body into the leg (shin splints), knee, lower back and hip. You may also experience inflammation (swelling, redness, heat and pain) along the inside of the ankle (along the posterior tibial tendon). Additionally, you may notice some changes in the way your foot looks. Your ankle may begin to turn inward (pronate), causing the bottom of your heel to tilt outward. Other secondary symptoms may also show up as the condition progresses, such as hammertoes or bunions. You may also want to check your footprint after you step out of the shower. (It helps if you pretend you?re in a mystery novel, and you?re leaving wet, footprinty clues that will help crack the case.) Normally, you can see a clear imprint of the front of your foot (the ball and the toes) the heel, and the outside edge of your foot. There should be a gap (i.e. no footprinting) along the inside where your arches are. If your foot is flat, it?ll probably leave an imprint of the full bottom of your foot-no gap to be had. Your shoes may also be affected: because the ankle tilts somewhat with this condition, the heel of your shoes may become more worn on one side than another.
Diagnosis
Podiatrists are trained in expertly assessing flat feet and identifying different risk factors and the causes for it. Initial assessment will begin with a detailed history attempting to find out if any underlying illness has resulted in this. A detailed clinical examination normally follows. The patient may be asked to perform certain movements such as walking or standing on their toes to assess the function of the foot. Footwear will also be analysed to see if there has been excessive wear or if they are contributing to the pronation of the foot. To assess the structure of the foot further, the podiatrist may perform certain x-rays to get a detailed idea of the way the bones are arranged and how the muscle tissues may be affecting them. It also helps assess any potential birth defects in a bit more detail.
pes planus radiology
Non Surgical Treatment
If you have flat feet, you may also experience pain throughout the lower body and into the lower back. Orthotics (custom-made rigid foot supports) can be prescribed when over-the-counter supports do not provide releif and surgery can also offer a more permanent solution in severe cases. The board-certified doctors in our practice would be able to select the most appropriate course of action in each case.
Surgical Treatment

Surgical procedures for flat feet vary depending on the root cause of the condition. Surgical correction to control pronation may include bone implants or Achilles tendon lengthening. Tendon transfer, which is a procedure to re-attach a tendon to another area of bone, may also be used to reduce pronation and improve foot function.
Prevention
Well-fitted shoes with good arch support may help prevent flat feet. Maintaining a healthy weight may also lower wear and tear on the arches.



 Morton's Neuroma is a common problem in runners, and there are a number of simple fixes you can try before resorting more drastic solutions like sclerosing or surgery. A Morton's Neuroma normally causes a burning pain in the forefoot, just behind the 3rd and 4th toes (sometimes behind the 2nd and 3rd toes). The pain often radiates towards the toes, and sometimes there is numbness rather than pain. The underlying cause is inflammation of the nerve between the bones of the forefoot, often triggered by narrow or tight shoes. I have had good results with the simple fixes described below, and I have had reports of other runners with similar success.
Morton's Neuroma is a common problem in runners, and there are a number of simple fixes you can try before resorting more drastic solutions like sclerosing or surgery. A Morton's Neuroma normally causes a burning pain in the forefoot, just behind the 3rd and 4th toes (sometimes behind the 2nd and 3rd toes). The pain often radiates towards the toes, and sometimes there is numbness rather than pain. The underlying cause is inflammation of the nerve between the bones of the forefoot, often triggered by narrow or tight shoes. I have had good results with the simple fixes described below, and I have had reports of other runners with similar success.




 Overview
Overview Symptoms
Symptoms Prevention
Prevention Hallux abductovalgus (HAV) or bunion, is a commonly seen deformity of the first metatarsophalangeal joint (MPJ) in which the hallux is abducted and everted, frequently overriding the second toe. Although the terms HAV and bunion are often used synonymously (as is done in this paper), it should be noted that a bunion actually refers to the callus and inflamed adventitious bursa overlying the HAV deformity. Even though bunions have been described in the medical literature for several hundred years (the word bunion is believed to be derived from the Latin, bunio, meaning turnip), there continues to be much controversy concerning its etiology. This is most likely because the development of HAV is multifactorial, stemming from a variety of structural and functional aberrancies.
Hallux abductovalgus (HAV) or bunion, is a commonly seen deformity of the first metatarsophalangeal joint (MPJ) in which the hallux is abducted and everted, frequently overriding the second toe. Although the terms HAV and bunion are often used synonymously (as is done in this paper), it should be noted that a bunion actually refers to the callus and inflamed adventitious bursa overlying the HAV deformity. Even though bunions have been described in the medical literature for several hundred years (the word bunion is believed to be derived from the Latin, bunio, meaning turnip), there continues to be much controversy concerning its etiology. This is most likely because the development of HAV is multifactorial, stemming from a variety of structural and functional aberrancies.